Home / Blog / What Causes Migraines in Females? Key Triggers, Hormonal Factors, and Prevention Tips
Migraine is a debilitating neurological condition that affects millions of women worldwide. In comparison to men, women experience migraines three times more often because of their biological and hormonal features. Migraine refers to a severe pulsating headache that is usually followed by vomiting, visual problems, and discomfort due to bright light or loud noise. For better quality of life, it is important to know the causes of migraines in women as well as appropriate prevention strategies for them.

Various factors, including hormone changes and lifestyle choices, can trigger migraine episodes in women. Common examples of migraine triggers in women include hormonal changes, inherited factors, stress, food, and surroundings.
It is possible to control and avoid attacks of migraine by recognising such triggers or risk factors and adopting necessary prevention strategies.
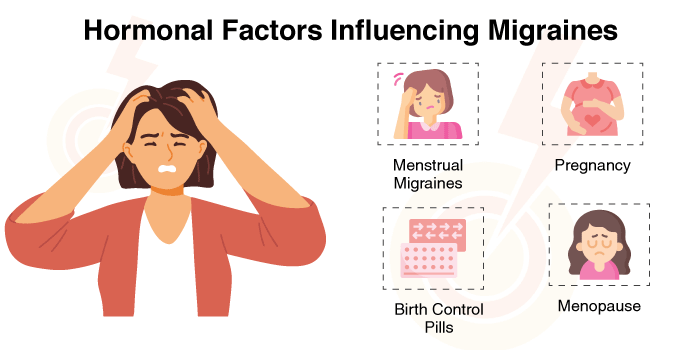
The reason why women get migraines more often than men is because of the hormonal changes they experience. There is a strong link between migraine and oestrogen, which is a principal hormone in women. A change, especially a quick reduction in the level of oestrogen, can lead to a migraine attack.
Some specific hormonal influences include:
Migraine is also partly genetic. Research shows that having a parent or brother/sister with migraines makes one highly susceptible to the condition. This means that some genes may be responsible for determining how an individual feels pain as well as what kind of stimulants can cause headaches for him or her.
Although migraines can be challenging to manage, several preventive measures can help reduce their frequency and severity:
Several lifestyle habits and environmental factors can also contribute to migraine in females. These include:
Migraine in females is affected by hormones, genes, and lifestyle factors. One can reduce their migraine risks by learning the common causes and specific triggers, like changes in hormones, stress, and eating certain foods, as well as surrounding factors; this can help women manage their migraine more effectively. Women can make sure that migraines do not affect them much during their daily lives if they take precautions like staying healthy, dealing with tension, and recognising what specifically causes their migraines.
For persistent or severe migraines, seeking medical advice from a healthcare professional is essential. If you are struggling with migraines, consider consulting experts at HCG Hospitals for specialised migraine treatment and migraine remedies. Taking proactive steps today can help lead to a healthier, migraine-free future.
Abrupt changes in estrogen levels are found to have a close association with migraine occurrence in women.
Hormonal changes seen before and during menstruation, during ovulation, after childbirth, and during perimenopause or menopause, along with hormonal changes that occur due to birth control pills or hormone therapy, can trigger migraine episodes in women.
Because hormone levels are constant during pregnancy, many women report that their migraines get better, especially in the second and third trimesters. Some women may have migraine episodes throughout their pregnancy.
In such cases, women must pay attention to:
Migraines can be less frequent and less intense with simple lifestyle changes:
Typically, migraines are more than just a typical headache.
Common symptoms of migraine include pain that worsens when there is movement or intense light; throbbing pain, usually on one side; extreme sensitivity to light and sound; nausea and vomiting; vision problems; and more.
Sinus headaches result in congestion and pressure in the face, whereas tension headaches typically feel like a tight band around the head.
Usually, migraines in women can be managed with home remedies, such as rest, hydration, and stress management. However, in some cases, women should see a doctor, especially if they experience the following signs and symptoms:
In such cases, doctors will recommend appropriate treatments, which may include trigger identification and management, medication, and more.
When under stress, the body releases stress hormones, adrenaline and cortisol, which narrow blood vessels and change pain pathways. Chronic stress can cause a severe imbalance in these hormone levels, leading to migraine.
Stress can also lead to estrogen imbalance, which can increase migraine risk.
Adopting stress-reduction strategies like mindfulness, breathing exercises, or relaxation therapy can help in preventing migraine attacks or reducing their frequency.
Migraines may be triggered by eye strain, bad posture, and exposure to bright or flickering light, all of which are brought on by prolonged screen use.
You can consider the following measures to reduce the risk of screen time-induced migraine: