Introduction to Migraines in Females
Migraine is a debilitating neurological condition that affects millions of women worldwide. In comparison to men, women experience migraines three times more often because of their biological and hormonal features. Migraine refers to a severe pulsating headache that is usually followed by vomiting, visual problems, and discomfort due to bright light or loud noise. For better quality of life, it is important to know the causes of migraines in women as well as appropriate prevention strategies for them.
Key Triggers of Migraines in Females

Various factors, including hormone changes and lifestyle choices, can trigger migraine episodes in women. Common examples of migraine triggers in women include hormonal changes, inherited factors, stress, food, and surroundings.
It is possible to control and avoid attacks of migraine by recognising such triggers or risk factors and adopting necessary prevention strategies.
What Causes Migraines in Females?
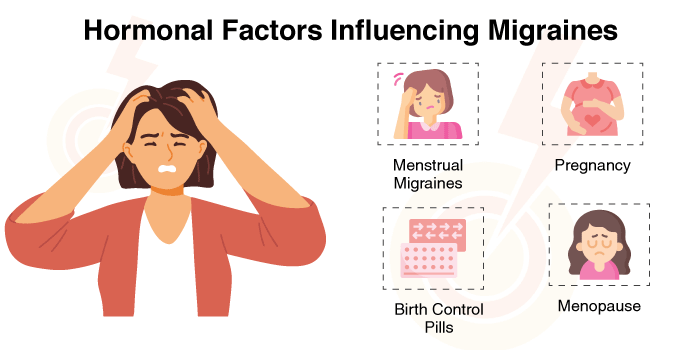
Hormonal Factors Influencing Migraines
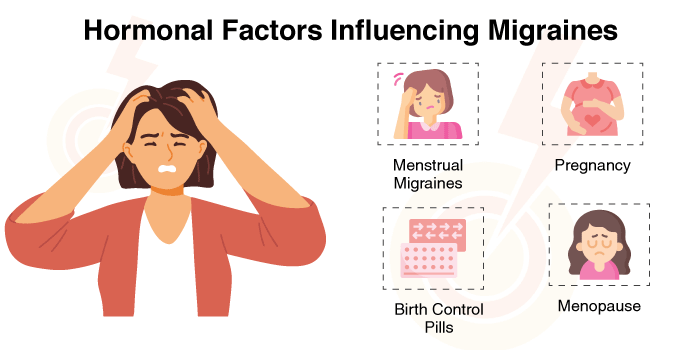
The reason why women get migraines more often than men is because of the hormonal changes they experience. There is a strong link between migraine and oestrogen, which is a principal hormone in women. A change, especially a quick reduction in the level of oestrogen, can lead to a migraine attack.
Some specific hormonal influences include:
- Menstrual Migraines: The reason behind migraines in most women is that the level of oestrogen decreases either before or during menstruation.
- Pregnancy: Some women get better from migraine, but others may have an aggravation, particularly in the first three months of pregnancy.
- Birth Control Pills: The use of hormonal contraceptives may either control or induce migraines among females according to their levels of oestrogen.
- Menopause: A lot of females undergoing menopause claim to have higher migraines owing to changing oestrogen levels, while others may experience relief post-menopause.
Genetics and Family History
Migraine is also partly genetic. Research shows that having a parent or brother/sister with migraines makes one highly susceptible to the condition. This means that some genes may be responsible for determining how an individual feels pain as well as what kind of stimulants can cause headaches for him or her.
Prevention Tips for Migraines in Females
Although migraines can be challenging to manage, several preventive measures can help reduce their frequency and severity:
- Keep a Regular Sleep Pattern: Failure to get enough sleep or sleeping at odd times may start a migraine. Try to sleep for 7-9 hours every night and make sure it is good sleep.
- Handle Stress Well: Migraine is mostly caused by stress. Consider practicing relaxation methods like meditation, yoga, breathing exercises, etc.
- Take Enough Water: Migraine can occur due to dehydration. Taking at least eight glasses of water per day may prevent attacks.
- Eat a Healthy Diet: Do not eat foods that are known to increase the risk of migraines, e.g., processed meat, caffeine, alcohol, and artificial sweeteners. Consume whole foods, fruits, and vegetables.
- Exercise Regularly: Migraines can occur less often if one engages in mild exercises like walking, swimming, or yoga.
- Reduce Exposure: Watching too much TV/computer light, especially blue light, may harm your eyes and cause migraines.
- Monitor Migraine Causes: A diary for recording migraines may reveal what brings them on and so can help in identifying the triggers and thereby reducing the frequency of migraine episodes.
- Consult a Doctor: If the migraine episodes are frequent and intense, it is advisable to see a doctor who may recommend effective migraine treatment options.
Lifestyle Factors Contributing to Migraines
Several lifestyle habits and environmental factors can also contribute to migraine in females. These include:
- Dietary Triggers: Food and drinks like caffeine, alcohol, junk food, and artificial sweeteners may cause migraines in a few females.
- Irregular Sleep Patterns: Sleeping too little or too much can bring on a migraine.
- Dehydration: Not drinking enough water may result in a headache or migraine.
- Excessive Screen Time: Spending many hours using electronic devices may cause eye fatigue as well as trigger migraines.
- Variations in the Weather: Abrupt changes in weather, such as very high moisture, intense sunshine, or rainstorms, can act as triggers.
- Pungent Smells and Noise Pollution: For sensitive people, mists, cigar fumes, and other strong vapours or smells may cause migraines.
- Stress and Anxiety: Chronic stress and anxiety are also identified as the main factors that can cause and worsen the occurrence of migraines.
- In such cases, patients should be promptly taken to a doctor for a detailed evaluation.
Conclusion
Migraine in females is affected by hormones, genes, and lifestyle factors. One can reduce their migraine risks by learning the common causes and specific triggers, like changes in hormones, stress, and eating certain foods, as well as surrounding factors; this can help women manage their migraine more effectively. Women can make sure that migraines do not affect them much during their daily lives if they take precautions like staying healthy, dealing with tension, and recognising what specifically causes their migraines.
For persistent or severe migraines, seeking medical advice from a healthcare professional is essential. If you are struggling with migraines, consider consulting experts at HCG Hospitals for specialised migraine treatment and migraine remedies. Taking proactive steps today can help lead to a healthier, migraine-free future.